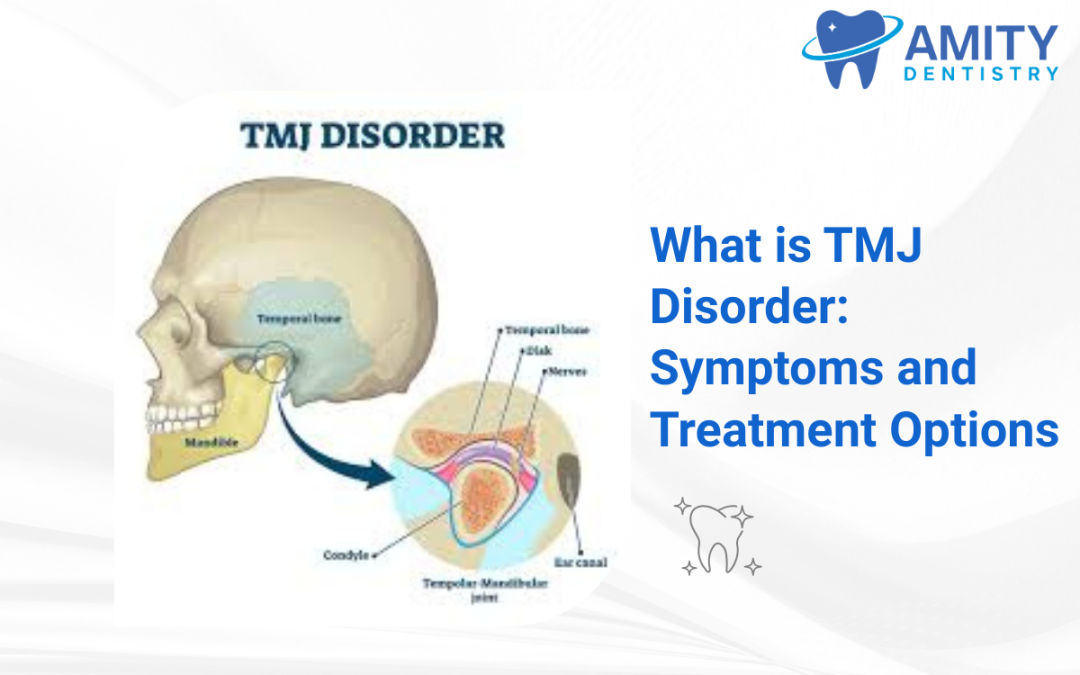
Your jaw joint is one of the most complex joints in your body. It is called the temporomandibular joint, or TMJ. You have one on each side of your face, just in front of your ears. This joint connects your lower jawbone, the mandible, to your skull. It is responsible for the many movements you need for daily life. Talking, chewing, and yawning all depend on a healthy, functioning TMJ.
When this intricate system of muscles, ligaments, and bone works incorrectly, it can cause significant pain and discomfort. This group of conditions is known as a TMJ disorder, or TMD. A TMJ disorder can affect the joint itself or the muscles that control its movement. Jaw pain is a very common symptom, but the condition can also cause headaches, earaches, and other issues. Many people live with these symptoms without understanding their source.
Getting a proper diagnosis is the first step toward relief. This guide will explain the symptoms and common causes of TMJ disorder. It will also detail the effective TMJ treatment options available through professional dental care. Understanding this condition is key to finding a lasting solution.
What is the Temporomandibular Joint?
To understand a TMJ disorder, you first need to understand the joint itself. The temporomandibular joint is a sophisticated structure. It allows your jaw to move in multiple directions. It acts as a sliding hinge. This dual motion allows you to open and close your mouth and to move your jaw from side to side.
The main components of the joint are the condyle and the temporal bone. The condyle is the rounded end of your lower jaw. It fits into a socket in the temporal bone of your skull. Between these two bones is a small piece of cartilage called the articular disc. This disc acts as a shock absorber and a cushion. It allows the joint to move smoothly and without friction. When you open your mouth, the disc glides forward with the condyle.
A complex group of muscles surrounds and supports the TMJ. These muscles control all the movements of your jaw. They are responsible for the powerful forces needed for chewing. A TMJ disorder occurs when any part of this system, the bones, the disc, or the muscles, is not working correctly. The term TMD is a broad label for a variety of problems that cause pain and dysfunction in this area. The goal of TMJ treatment is to identify the source of the dysfunction and restore harmony to the system.
Common Symptoms of TMJ Disorder
A TMJ disorder presents a wide range of symptoms. These symptoms can be confusing because they often appear in areas other than the jaw. This is why the condition is sometimes misdiagnosed. Recognizing the full spectrum of symptoms is important for getting the right help.
The most direct symptoms relate to the jaw itself. Persistent jaw pain or tenderness is the most common complaint. This pain is usually located in the area just in front of the ear. It may affect one or both sides of your face. You might feel a dull, aching pain that worsens with jaw movement. Chewing food can become difficult or painful. In some cases, the jaw joint can lock. This makes it hard to fully open or close your mouth. This locking can be temporary or may require manual manipulation of the jaw to resolve.
Sounds coming from the jaw joint are also a very common sign. You might hear a clicking, popping, or grating sound when you open your mouth or chew. It is important to note that jaw sounds without any associated pain or limited movement are not always a sign of a TMJ disorder. Many people have jaw sounds with no other issues. When these sounds are accompanied by pain, however, it usually indicates a problem with the position of the articular disc.
A TMJ disorder often causes referred pain. This is pain that is felt in a location other than its source. Frequent headaches, especially those that feel like tension headaches, are a common symptom. The constant strain in the jaw muscles can radiate to the muscles in the temples and forehead. You may also experience neck and shoulder pain. The muscles of the jaw and neck are interconnected, so tension in one area can easily spread to the other. Earaches, a feeling of fullness in the ears, and tinnitus, or ringing in the ears, are also linked to TMJ issues. Other symptoms include a tired feeling in the face or the sensation that your upper and lower teeth do not fit together correctly.
What Causes TMJ Disorder?
The exact cause of a person’s TMJ disorder can be difficult to pinpoint. In most cases, the problem is the result of several contributing factors rather than a single cause. These factors can relate to the joint itself, the surrounding muscles, or the alignment of your teeth.
Problems directly within the joint are a common source of TMD. The articular disc can move out of its proper alignment or erode over time. This reduces the joint’s cushioning and causes the bones to grind against each other. The cartilage within the joint can also be damaged by arthritis. Both osteoarthritis and rheumatoid arthritis can affect the temporomandibular joint, leading to inflammation and degeneration. A direct injury to the jaw, such as from an impact or accident, can also damage the joint and lead to long-term problems.
Muscle issues are another major contributor to TMJ disorder. Myofascial pain, which is pain in the muscles and their connective tissues, is very common. The primary cause of this muscle strain is often bruxism. Bruxism is the medical term for the chronic, involuntary grinding or clenching of teeth. Many people do this in their sleep without being aware of it. This habit places an enormous amount of force on the jaw muscles and the TMJ. This leads to muscle fatigue, inflammation, and pain.
Stress is also a significant factor. When you are under stress, you may unconsciously tighten your facial and jaw muscles. This constant tension contributes to the same muscle fatigue and pain associated with bruxism. Finally, your bite, or occlusion, can play a role. If your teeth do not fit together correctly, it can place your jaw in an unnatural position. This misalignment can strain the joint and muscles over time. A bad bite, known as malocclusion, or missing teeth can disrupt the balance of your jaw system.
How a Dentist Diagnoses TMJ Disorder
If you are experiencing jaw pain or other related symptoms, a dentist with experience in TMJ treatment is the right professional to see. The diagnostic process is thorough. It is designed to identify the specific source of your problem.
Your appointment will begin with a detailed discussion of your symptoms. Your dentist in Charlotte NC will ask you about the location, frequency, and intensity of your pain. They will ask about any jaw sounds you hear and any difficulty you have with jaw function. They will also discuss your medical history and lifestyle factors. This includes asking about your stress levels, sleep habits, and any potential injuries. This conversation provides important clues about the potential causes of your condition.
Next, your dentist will conduct a physical examination of your jaw and head. They will ask you to open and close your mouth and move your jaw from side to side. During these movements, they will observe your jaw’s range of motion. They will listen for any clicking or grating sounds. The dentist will then gently press on different areas of your face, jaw, and neck. This is done to identify specific points of pain or tenderness in the muscles and around the joint itself.
Your dentist will also perform a bite analysis. They will look at how your upper and lower teeth fit together. They will check for signs of wear on your teeth, which is a strong indicator of bruxism. In some cases, imaging may be needed to get a more detailed view of the joint. A panoramic X-ray can show the bony structures of the jaw. For a more detailed look at the soft tissues, including the articular disc, a CT scan or an MRI might be recommended.
Professional TMJ Treatment Options
After a thorough diagnosis, your dentist can recommend a treatment plan. The goal of TMJ treatment is to relieve your pain, restore normal function, and prevent the problem from recurring. The approach to dental care for TMJ disorder almost always begins with the most conservative and reversible treatments.
One of the most effective and common treatments is the use of an oral appliance. These are also known as splints or night guards. An oral appliance is a custom-fitted device made of hard acrylic. It is designed to be worn over your upper or lower teeth, usually at night. A custom appliance made by a dentist is very different from a boil-and-bite guard you can buy at a chemist. A professional appliance is precisely fabricated to fit your mouth.
These devices have two main functions. First, they create a physical barrier between your upper and lower teeth. This protects your teeth from the damaging forces of grinding and clenching. Second, and more importantly for TMJ pain, the appliance is designed to place your jaw in a more relaxed and orthopedically stable position. This reduces tension in your jaw muscles and decreases the pressure on your temporomandibular joint. For many patients, wearing a custom splint provides significant pain relief.
If your TMJ disorder is related to a problem with your bite, your dentist in Charlotte might recommend occlusal adjustments. This involves making very slight and precise modifications to the chewing surfaces of your teeth. By selectively reshaping a few high spots, the dentist can help your teeth fit together more evenly. This can balance the forces on your jaw and relieve strain. In cases of more severe malocclusion, orthodontic treatment with braces may be needed.
Restoring your mouth to a stable condition is also important. If you have missing teeth or heavily worn teeth, your bite can become unbalanced. Using dental crowns, bridges, or implants to restore your teeth can improve the alignment of your jaw. This helps to distribute chewing forces evenly. In many cases, a comprehensive TMJ treatment plan will involve a combination of these approaches.
Conclusion
You do not need to endure the persistent discomfort of a TMJ disorder. The chronic jaw pain, headaches, and other symptoms associated with this condition are treatable. Ignoring the problem can lead to worsening pain and further damage to your jaw joint and teeth. The correct path to relief starts with a proper diagnosis from a dental professional. Your dentist can help identify the underlying causes of your condition.
A professional dentist in Pineville plan offers a range of effective and non-invasive solutions to manage your symptoms. From custom-fitted oral appliances to precise bite adjustments, these treatments are designed to restore comfort and proper function to your jaw. Taking action is the first step toward a life free from jaw pain.
You do not have to live with chronic jaw pain. At Amity Dentistry, we provide a thorough diagnosis for TMJ disorder. We offer a range of effective TMJ treatment options, including custom-fitted oral appliances. Our goal is to relieve your pain and restore proper jaw function. Want a trusted Charlotte dentist for your smile? Schedule your appointment at 980-423-1244 and Book Now without delay.